1. Metabolic
The GIT microbiota is involved in multiple aspects of our metabolism, for example, by producing essential nutrients (such as vitamins K2 and B12, folate, amino acids and fatty acids) and extracting energy from fibre. In fact, vegetables, nuts and fruits have a fair amount of non-digestible fibre (dietary fibre) that reaches the large intestine mainly intact. Once there, the microbiota can take advantage of dietary fibre and generate energy from it, producing waste products such as short-chain fatty acids. Those acids can be used as an energy source by GIT cells and help to maintain a healthy pH, which inhibits the growth of some pathogens. For instance, butyrate is one of the most relevant short-chain fatty acid produced by the intestinal microbiota. Besides being an energy source for the colon, it has anti-inflammatory and immunomodulatory properties (2).
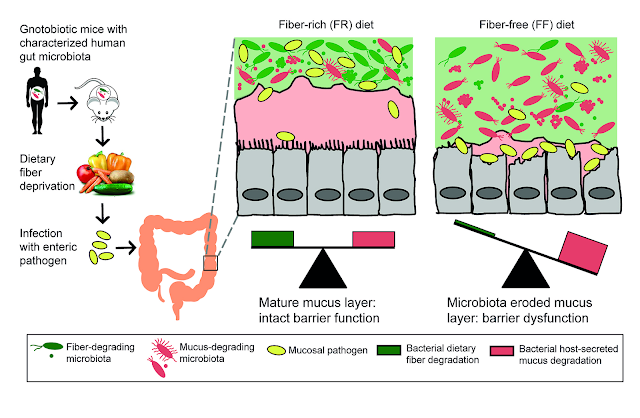 |
| Figure 1 — A fibre-rich versus a fibre-deprived gut microbiota (10). |
2. Structural and Protective
The GIT prevents potential pathogenic microorganisms from adhering to its cells, as it establishes an extensive surface coating in the epithelium and may produce antimicrobial compounds (such as bacteriocins and acids). Additionally, the immune cells of the GIT secrets roughly 60% of the human body immunoglobulins, in the vast gut-associated lymphoid tissue (GALT), that has a strong relationship with the microbiota (3,4). Although countless beneficial interactions have been established between GIT immune cells and GIT microbiota, the majority may remain uncertain or unknown.
3. Maturation of Innate and Adaptive Immune Responses
It is also very significant to help the immune system distinguishing commensal from undesirable microorganisms (5). Commensal GIT microbes can interact with the immune system and induce regulatory T cells, that balances the host Th1 and Th2 immune responses, which dysregulation may lead to autoimmune and atopic diseases, respectively (6,7). Therefore, a healthy GIT microbiota may play a significant role in diminishing the prevalence and symptomatology of autoimmune disorders and allergies.
4. Physical and Psychological Health
In the last decade, the GIT microbiota has been closely associated with the global health of its host. For example, multiple cases of autism have been related to disturbs of the microbiota, principally due to a prolongated intake of antibiotics in the first years of life and Clostridium enteric infections (8). The GIT microbiota has also been linked to variation in moods and emotions by excreting neurotransmitters into the bloodstream, such as noradrenaline and serotonin by certain strains of Escherichia coli. The microbiota-gut-brain axis is one of the most complex and least know interactions to date and can be closely related to mood disorders, which affects 10% of the world’s population. Therefore, the GIT microbiota emerges as a potential therapeutic and diagnose target to treat such disorders in the future (9).
REFERENCES
- O’Hara AM, Shanahan F. The gut flora as a forgotten organ. EMBO Rep. 2006;7(7):688-693. doi:10.1038/sj.embor.7400731
- Liu H, Wang J, He T, et al. Butyrate: A double-edged sword for health? Adv Nutr. 2018;9(1):21- 29. doi:10.1093/advances/nmx009
- Arrazuria R, Pérez V, Molina E, Juste RA, Khafipour E, Elguezabal N. Diet induced changes in the microbiota and cell composition of rabbit gut associated lymphoid tissue (GALT). Sci Rep. 2018;8:14103. doi:10.1038/s41598-018-32484-1
- Brandtzaeg P, Halstensen TS, Kett K, et al. Immunobiology and immunopathology of human gut mucosa: Humoral immunity and intraepithelial lymphocytes. Gastroenterology. 1989;97:1562-1584. doi:10.1016/0016-5085(89)90406-X
- Montalto M, D’Onofrio F, Gallo A, Cazzato A, Gasbarrini G. Intestinal microbiota and its functions. Dig Liver Dis Suppl. 2009;3(2):30-34. doi:10.1016/S1594-5804(09)60016-4
- Azad MB, Kozyrskyj AL. Perinatal programming of asthma: The role of gut microbiota. Clin Dev Immunol. 2012;2012:932072. doi:10.1155/2012/932072
- Skapenko A, Leipe J, Lipsky PE, Schulze-Koops H. The role of the T cell in autoimmune inflammation. Arthritis Res Ther. 2005;7(Suppl 2):S4-14. doi:10.1186/ar1505
- Collen A. 10% Humanos. 1st ed. Lisboa: Objectiva Editora; 2016. https://www.wook.pt/livro/10-humanos-alanna-collen/17436036.
- Huang TT, Lai JB, Du YL, Xu Y, Ruan LM, Hu SH. Current understanding of gut microbiota in mood disorders: An update of human studies. Front Genet. 2019;10:98. doi:10.3389/fgene.2019.00098
- Desai MS, Seekatz AM, Koropatkin NM, et al. A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility. Cell. 2016 Nov 17;167(5):1339-1353.e21. doi: 10.1016/j.cell.2016.10.043. PMID: 27863247; PMCID: PMC5131798







Sem comentários:
Enviar um comentário